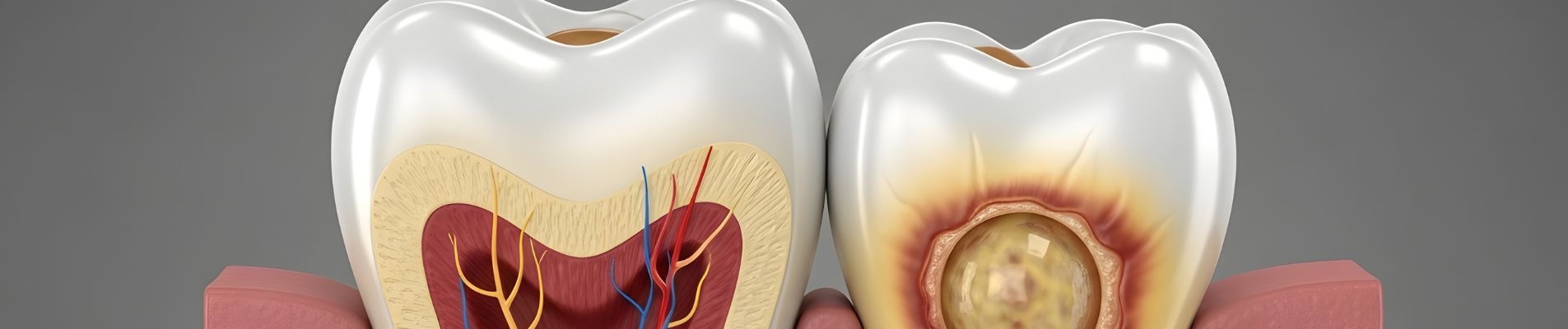
A tooth abscess is a pocket of pus that forms when bacteria infect the tissue inside or around a tooth. It typically develops at the root tip or along the gum line, creating pressure, swelling, and often intense pain. Many patients experiencing this discomfort turn to the internet and search: can you burst a tooth abscess?
The build-up of pus inside the abscess creates significant pressure against surrounding tissue. This is what causes the throbbing sensation many people describe. As the pocket grows, the pain can spread across the jaw, ear, and neck. Understandably, patients look for quick relief — and some consider popping it themselves.
The good news is that effective, safe treatment is available. A dental professional can drain the infection properly, address the underlying cause, and help you recover fully. Understanding what an abscess is — and what not to do — is the first step towards getting the right care.
Experiencing these symptoms?
Delaying treatment can lead to tooth loss. We have slots available today.
Can You Burst a Tooth Abscess Safely?
Direct answer: No, you should not try to burst a tooth abscess yourself. Self-drainage spreads bacteria into surrounding tissue, increases the risk of deeper infection, and does not remove the source of the problem. Only a dentist can safely drain an abscess and treat the underlying cause. Pain relief after a rupture is always temporary.
When patients ask "can you burst a tooth abscess," the answer is always the same: it is not safe to do so at home. The pus inside the abscess contains live bacteria. Squeezing, piercing, or pressing on the swelling pushes these bacteria deeper into the tissue and sometimes into the bloodstream.
Even if the abscess seems to drain and you feel immediate relief, the source of infection remains inside the tooth or gum. Without professional treatment, the infection will return — often worse than before. Temporary pain reduction tricks people into thinking the problem has resolved, but the bacteria continue to multiply beneath the surface.
Meet Dr. Yasha Shirazi
Principal Dentist at Emergency Dentist London
"We treat hundreds of dental emergencies every month. The sooner you come in, the easier the fix usually is."
Book an appointment with our team →Self-drainage carries several specific risks:
- Infection spread — Bacteria can travel to the jaw bone, throat, or soft tissue spaces in the neck
- Deeper tissue involvement — Pressing on the abscess may force pus into tissue planes where it becomes harder to treat
- Delay in proper treatment — Feeling temporary relief often causes patients to postpone the dental visit they genuinely need
If you are in pain from a suspected abscess, the safest step is to contact a dentist for an urgent assessment rather than attempting anything at home.
What Happens If a Dental Abscess Burst in the Mouth?
Sometimes a dental abscess burst happens on its own, without any interference. The pressure inside the pocket builds until the wall of the abscess gives way, releasing pus into the mouth. You may notice a sudden foul taste, a rush of salty or bitter fluid, and almost immediate reduction in pain.
This experience can feel like a relief. The throbbing stops, the swelling goes down, and it seems as though the problem has sorted itself out. Unfortunately, that is not the case. An abscess rupture in mouth only releases the built-up pus — it does nothing to address the infected tissue or decayed tooth that caused the abscess in the first place.
After a burst abscess in mouth, the drainage tract often closes over within a day or two. Pus begins to collect again because the bacteria are still active at the root or gum. Many patients go through repeated cycles of swelling, bursting, and temporary relief before finally seeking professional help.
An abscessed tooth rupture — whether it happens naturally or is caused by pressure — leaves the infection source untouched. Bursting tooth abscess does not equal treatment. The bacteria responsible for the abscess remain inside the tooth canal or periodontal pocket, continuing to destroy tissue and bone over time.
Signs that a dental abscess has ruptured include:
- A sudden bad taste in the mouth
- Pus or fluid draining from the gum near the affected tooth
- A noticeable decrease in pain and pressure
- A small bump on the gum that appears to have opened
Even after natural drainage, professional assessment is still essential to clear the infection and prevent recurrence.


Real Patient Result: Emergency White Filling
Treatment by Dr Kamran
Can You Pop a Dental Abscess at Home?
Searching online for "can you pop a dental abscess" returns thousands of results, some of which suggest home drainage methods. These approaches are unsafe, regardless of how carefully they are described. A dental abscess pop using a needle, pin, or any sharp household object introduces new bacteria into the wound and risks puncturing tissue that should not be disturbed.
Attempting a gum abscess pop at home is particularly risky because the tissues in the mouth are richly supplied with blood vessels. A puncture wound in the gum can bleed heavily, become infected with additional bacteria from the object used, and cause damage to nerves and surrounding structures.
Popping tooth abscess at home also creates a false sense of security. The released pus makes the area feel better temporarily, but within hours or days the infection builds again. Meanwhile, bacteria may have spread to areas that were previously unaffected.
There are clear reasons why DIY attempts make things worse:
- Non-sterile instruments introduce additional bacteria into an already infected site
- Sharp objects can damage healthy tissue, blood vessels, and nerves nearby
- Incomplete drainage leaves bacteria behind to multiply and reform the abscess
- Delayed treatment allows the infection to progress further before professional care begins
If you feel tempted to drain the swelling yourself, it is a strong indicator that you need professional help promptly. The discomfort driving that urge is exactly what a dentist is trained to resolve safely.
Can Popping a Gum Abscess Kill You?
This is a question many worried patients ask, and it deserves a factual, balanced answer. In extremely rare cases, an untreated dental infection can spread to critical areas such as the throat, chest, or bloodstream. When this happens, the condition can become very serious. So when patients ask "can popping a gum abscess kill you," the honest answer is that the infection behind the abscess — if left completely untreated — carries genuine risks.
However, context matters. The vast majority of dental abscesses are treatable, especially when patients seek care early. Life-threatening complications from a dental root infection are rare and typically occur after prolonged neglect, not from a single event. Popping the abscess itself is not what creates the danger — it is the ongoing, untreated infection that poses the real risk.
The important message is that untreated dental infection can progress. Bacteria from a dental root infection may spread to soft tissue spaces in the neck, causing swelling that compromises breathing. In exceptional circumstances, infection can enter the bloodstream. These outcomes are preventable with timely professional drainage and appropriate treatment.
Rather than worrying about worst-case scenarios, the practical step is to have the abscess assessed by a qualified dentist. Professional drainage under sterile conditions, combined with treatment of the infection source, resolves the problem safely in the overwhelming majority of cases.
Will a Tooth Abscess Go Away With Antibiotics?
Many patients hope that antibiotics alone will resolve an abscess without further treatment. The question "will a tooth abscess go away with antibiotics" comes up frequently, and the answer is usually no — not completely.
Antibiotics can reduce the bacterial load and help control the spread of infection. They are useful when prescribed alongside dental treatment, particularly when there is facial swelling, a raised temperature, or signs that infection is spreading. However, antibiotics cannot reach the source of the problem.
The infection originates inside the tooth — either within the nerve canal or at the root tip. Antibiotics travel through the bloodstream, but they cannot penetrate dead tissue inside a tooth effectively. The bacteria sheltered within the root canal remain protected and continue to produce toxins that sustain the abscess.
This is why a dental root infection requires physical removal of the source. Whether that means root canal treatment to clean and seal the infected canal, or extraction of a tooth that cannot be saved, the cause of the infection must be addressed directly. Antibiotics play a supporting role, but they are not a standalone cure.
Relying on repeated courses of antibiotics without treating the tooth itself leads to recurring infections, antibiotic resistance, and progressive bone loss around the root. The most effective approach combines professional drainage with definitive treatment of the tooth.
Abscess After Root Canal — Why Does It Happen?
An abscess after root canal is frustrating, but it does occur in some cases. Root canal treatment aims to remove all infected tissue from inside the tooth and seal it permanently. When successful, it eliminates the infection and preserves the natural tooth. Occasionally, however, an abscess tooth on root canal can develop weeks, months, or even years later.
Several factors can contribute to this:
- Incomplete cleaning — Some teeth have complex canal systems with branches or curves. If a small amount of infected tissue is left behind, bacteria can regrow over time.
- Seal failure — The filling material placed inside the root canal may break down or develop a gap, allowing bacteria to re-enter the canal from above or below.
- New decay — A tooth that has had root canal treatment can still develop new decay around the crown or filling, creating a new pathway for bacteria to reach the root.
- Root fracture — A crack in the root of the tooth provides an entry point for bacteria, even if the canal itself was treated successfully.
When an abscess after root canal is suspected, the dentist will take an x ray tooth abscess image to assess the root, surrounding bone, and the quality of the existing root filling. This X-ray helps determine whether retreatment, a surgical approach, or extraction is the best option.
Retreatment is often successful, particularly when the original issue was incomplete cleaning rather than a structural problem with the tooth.
Abscess After Tooth Extraction — Is It Normal?
Developing an abscess after tooth extraction is not common, but it does happen. After a tooth is removed, the socket usually heals within a week or two. If bacteria enter the healing socket — through food debris, poor oral hygiene, or a pre-existing infection — an abscess can form at the extraction site.
Signs of a post-extraction infection include:
- Increasing pain several days after the extraction, rather than gradually improving
- Swelling that gets worse instead of settling down
- A bad taste or pus draining from the socket area
- A raised temperature
- Difficulty opening the mouth or swallowing
Mild soreness and slight swelling after an extraction are normal. What is not normal is worsening symptoms beyond the first two or three days. If swelling becomes more pronounced, spreads to the cheek or neck, or is accompanied by a fever, the extraction site should be reviewed promptly by a dentist.
Most post-extraction infections respond well to cleaning of the socket combined with a short course of antibiotics. Early assessment prevents the infection from spreading to adjacent tissue.
How Dentists Diagnose a Tooth Abscess
Diagnosing a tooth abscess involves a combination of clinical examination and imaging. The dentist will examine the affected area, checking for swelling, tenderness, and any visible drainage. Tapping on the tooth or applying gentle pressure to the gum often helps identify the source of infection.
An x ray tooth abscess image is one of the most useful diagnostic tools. The X-ray reveals whether infection has spread to the bone around the root tip, how extensive the damage is, and whether the tooth has any structural problems such as cracks or failed previous treatment. X-rays also help distinguish between a gum abscess and a tooth abscess, which require different treatment approaches.
Identifying a dental root infection accurately is essential because it determines the correct treatment plan. A gum abscess caused by trapped debris beneath the gum line is managed differently from an abscess originating inside the tooth canal. The clinical exam combined with imaging gives the dentist the full picture.
In some cases, additional tests such as vitality testing — which checks whether the nerve inside the tooth is alive or dead — help confirm the diagnosis. A dead nerve indicates that infection has destroyed the tissue inside the tooth and root canal treatment or extraction is needed.
Safe Treatment Options for a Tooth Abscess
Professional treatment is the only reliable way to resolve a tooth abscess. The approach depends on the location, severity, and cause of the infection. Your dentist will recommend the most appropriate option after examination and imaging.
Common treatment options include:
- Professional drainage — The dentist makes a small incision under local anaesthetic to drain the pus, relieve pressure, and clean the area. This provides immediate relief and removes the bacterial collection safely.
- Root canal treatment — If the infection originates inside the tooth, root canal treatment removes the infected nerve tissue, cleans and disinfects the canal system, and seals it to prevent reinfection. This preserves the natural tooth.
- Extraction — When a tooth is too damaged to save, removal may be the most appropriate option. Once the tooth is extracted, the infection source is eliminated and healing can begin.
- Pain management — Appropriate pain relief is provided throughout treatment. Over-the-counter painkillers can help manage discomfort while you wait for your appointment.
If you are experiencing severe toothache, do not wait for the problem to resolve on its own. Early treatment is simpler, faster, and far more comfortable than managing a long-standing infection. Our guide to dental abscess symptoms and treatment provides further detail on what to expect during care.
In cases involving dental trauma, an abscess may develop days or weeks after the initial injury. Prompt assessment helps prevent this complication. If you need urgent care without a prior appointment, our walk-in dentist service offers same-day access.
When a Tooth Abscess Becomes a Dental Emergency
Most tooth abscesses cause localised pain and swelling that can be managed with a timely dental appointment. However, certain signs indicate that the infection may be progressing beyond the tooth area, and same-day care becomes important.
You should seek urgent dental attention if you experience:
- Increasing swelling — Swelling that spreads from the gum to the cheek, under the jaw, or towards the eye area
- Difficulty swallowing — This may indicate the infection is affecting the throat area and needs prompt intervention
- Fever — A raised temperature alongside dental pain suggests the body is fighting a spreading infection
- Spreading redness — Red, warm skin extending beyond the immediate area of the tooth
- Difficulty breathing — Any change in breathing should be treated as an emergency
These symptoms do not mean every abscess becomes dangerous. They are simply indicators that professional assessment should happen sooner rather than later. Most infections respond well to prompt treatment, and complications are uncommon when care is received in good time.
If you notice any of these signs outside of regular hours, same-day emergency dental care is available. Acting early gives you the best possible outcome and avoids unnecessary discomfort.
Preventing Tooth Abscesses in the Future
While not every abscess is preventable, many develop from dental problems that could have been caught and treated earlier. Taking a few straightforward steps significantly reduces your risk.
- Treat cavities early — Small fillings prevent decay from reaching the nerve and causing an abscess. The longer a cavity is left, the more likely it is to progress to infection.
- Attend root canal follow-ups — If you have had root canal treatment, keep your follow-up appointments. Your dentist will check healing and the quality of the seal with X-rays.
- Maintain good oral hygiene — Brushing twice daily with fluoride toothpaste and cleaning between teeth removes plaque and bacteria before they cause damage.
- Book routine check-ups — Regular examinations allow your dentist to spot early signs of decay, gum disease, or cracks before they develop into infections.
- Do not delay symptoms — Persistent sensitivity, mild aching, or a small bump on the gum are all signs that something needs attention. Addressing these early is always easier than managing a full-blown abscess.
Prevention is always preferable to emergency treatment. A consistent routine of good oral care and regular professional check-ups provides the strongest protection against dental abscesses.
Frequently Asked Questions
Can you burst a tooth abscess?
No, you should not attempt to burst a tooth abscess yourself. The pus inside contains bacteria that can spread to surrounding tissue and potentially the bloodstream if disturbed improperly.
A dentist can drain the abscess safely under sterile conditions, ensuring the infection is properly managed and the source is treated. Self-drainage only provides temporary relief and leaves the underlying cause untouched.
If you are in pain from a suspected abscess, contact a dental professional for an urgent assessment rather than attempting to burst it at home.
Can you pop a dental abscess?
Popping a dental abscess at home is not safe. Using needles, pins, or other objects introduces additional bacteria and risks damaging healthy tissue, blood vessels, and nerves.
Professional drainage involves sterile instruments, local anaesthetic, and proper follow-up treatment. This approach resolves the infection effectively and prevents complications that home attempts can cause.
Can popping a gum abscess kill you?
In very rare circumstances, an untreated dental infection can spread to critical areas of the body and become life-threatening. However, this outcome is uncommon and almost always the result of prolonged neglect rather than a single event.
The risk is not from the act of popping itself, but from leaving the underlying infection completely untreated over an extended period. Seeking timely professional care prevents serious complications in the vast majority of cases.
Will a tooth abscess go away with antibiotics?
Antibiotics alone rarely cure a tooth abscess. They can help control the spread of infection and reduce swelling, but they cannot reach bacteria sheltered inside a dead tooth or sealed root canal.
The source of the infection must be treated directly — usually through root canal treatment or extraction. Antibiotics are most effective when used alongside professional dental treatment rather than as a standalone solution.
What happens if a dental abscess burst?
When a dental abscess bursts — either naturally or from pressure — you may notice a foul taste, pus drainage, and sudden pain relief. While the immediate discomfort reduces, the infection source remains inside the tooth or gum.
The drainage tract typically closes within a day or two, and pus begins to collect again. Professional assessment is still needed after a burst abscess to treat the cause and prevent the cycle from repeating.
Abscess after root canal — why does it happen?
An abscess can develop after root canal treatment if bacteria were not fully removed during the procedure, if the seal inside the canal breaks down, or if new decay develops around the treated tooth.
Complex root anatomy, fine canal branches, and root fractures can also contribute. Your dentist will use X-rays to assess the situation and may recommend retreatment, a surgical approach, or extraction depending on the findings.